Iodine and Your Thyroid: Understanding the Workings of This Butterfly-Shaped Gland
By Jennifer Wolff-Gillispie HWP, LC
Originally published by A Voice For Choice Advocacy on June 05, 2025.
“Your thyroid is like a delicate orchestra, and all the players need to be in harmony for optimal health.”
~ Anthony William, author of “Medical Medium Thyroid Healing.”
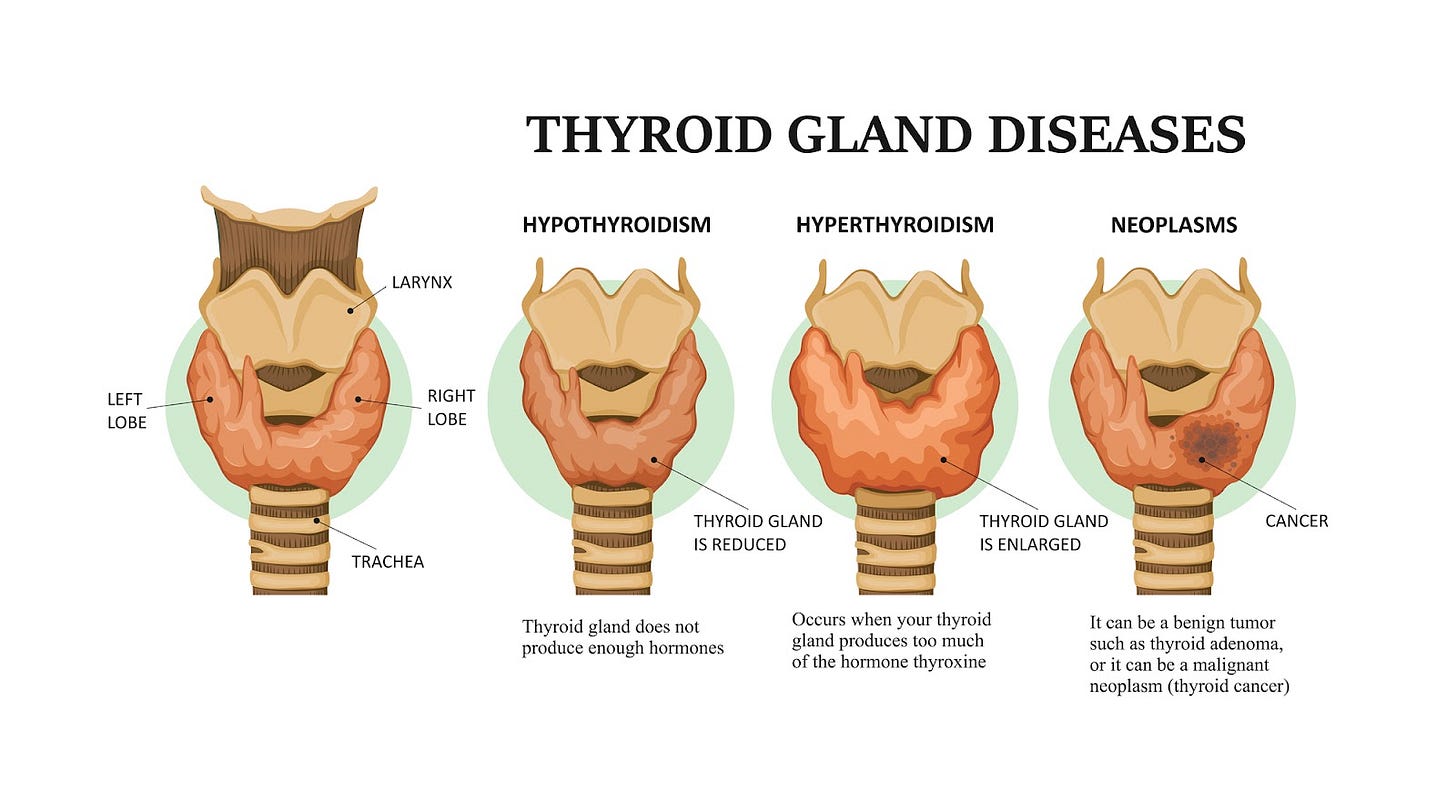
The thyroid—one of the smallest and most powerful glands in your body. It may not get as much attention as the heart or brain, but it is essential to nearly every physiological process. John E. Hall, Ph.D., professor and chair of Physiology and Biophysics at Arthur C. Guyton, exalts its importance in the Guyton and Hall Textbook of Medical Physiology, “Thyroid hormone increases the rates of most chemical reactions in all cells, thus helping to set the tempo of bodily activity.” Located in your neck, this organ has two lobes that extend to either side of your throat, releasing hormones that regulate metabolism, energy production, and mood. Despite its importance in keeping you going, thyroid disorders are becoming increasingly common. Millions of people worldwide suffer from the often exhausting and debilitating symptoms caused by thyroid dysfunction that cause conditions like hypothyroidism, hyperthyroidism, and autoimmune thyroid disease. A significant contributor to these dysfunctions is environmental toxins that you knowingly or unknowingly are exposed to, and dietary deficiencies, particularly with the mineral iodine. While research is proving that these factors play a part in thyroid dysfunction rates, there are actions you can take, as well as elements to avoid, to support a healthy thyroid.
Thyroxine (T4) and triiodothyronine (T3) are the two main hormones that your thyroid produces. These hormones play a crucial role in regulating metabolism, supporting growth and development, and controlling energy expenditure. While T3 is the usable/active form your body requires, your thyroid is only able to produce around 20% of it. The remaining amount your body needs must be converted from T4 into T3 through a process known as deiodination. During this process certain tissues (especially the liver) remove an iodine molecule from T4 to create the active form of T3. Iodine’s role in this process is indispensable, and it all starts with the foods you eat. Without adequate iodine, the thyroid cannot produce sufficient amounts of T3 and T4 hormones, leading to an imbalance that sabotages your body and inhibits normal physiological functioning. While iodine is essential for your thyroid to function, the body does not naturally produce it, so it must be obtained through dietary sources. Over 90% of the iodine you get from food is assimilated in the body as potassium iodide. Iodized salt, fortified foods, seafood, and dairy products are common sources of iodine, yet deficiency still affects over two billion people worldwide. Even with universal salt iodization programs across the globe that aim to add iodine to all salt used for human and animal consumption, there remains a huge percentage of the population at risk of being deficient, which can lead to unintended health consequences.
The Problem With Iodine Deficiency
One of these concerns is hypothyroidism. With this condition, a lack of dietary iodine results in reduced thyroid hormone production, leading to classic symptoms such as fatigue, weight gain, depression, and cold intolerance. Another condition to be aware of is a goiter. When iodine levels are insufficient, the thyroid enlarges in an attempt to compensate for its inability to produce sufficient hormones, and produces a lump in the throat. Children in and out of utero are at a risk of cognitive and developmental issues due to iodine deficiency. When they do not receive enough iodine, it can impair their growth and intelligence, a health problem known as cretinism. In addition to concerns about not getting enough iodine, it is also suggested by researchers that there is an increased risk of thyroid disorders from the very thing that was created to help with deficiencies—iodized salt. From the investigation, “Analysis of the correlation between high iodized salt intake and the risk of thyroid nodules: a large retrospective study,” that examined the data from patients that were given physicals at Third Xiangya Hospital of Central South University from 2017 to 2019, they found:
“... a daily intake of more than 5 g [one teaspoon] of iodized salt was not only an independent risk factor for the occurrence of thyroid nodules, but also an independent risk factor for the occurrence of thyroid cancer.”
That 5 grams of iodized salt (equal to 2000 mg of sodium) you may expect from an extra-large fast food “drive thru” meal, can just as easily be found in local diners, cafes, food trucks, and higher-end restaurants. According to Nielsen (a global data, statistics and analytics company), data showed 53% of salt sold in large chain and independent grocery stores was iodized. In a 2021 survey, “Share of households consuming iodized salt worldwide as of 2021, by select region,” 88.7% of the world population consumed iodized salt in their homes. This means that aunt Sally and grandma may still have that blue canister with a little girl and her umbrella in the cupboard, with the contents being added to your favorite dishes. “Iodized salt may cause hypertension,” a study conducted on 100 senior citizens, showed that regular use of iodized salt put them at higher risk for hypertension than those who opted for non-iodized (rock) salt. The research went on to claim that use of iodized salt disturbs the rhythm of the heart leading to heart disease, heart attack, and stroke.
While many academic institutions and well-meaning medical providers may encourage you to “halt the salt,” or advise on “how to reduce sodium in your diet,” the best advice is perhaps a little more nuanced. Should you avoid highly-processed foods that contain sodium additives that are not salt, including monosodium glutamate (MSG)? The answer is yes. Is it wise to avoid iodized salt (made from mining salt deposits and then processed)? Absolutely. Is all salt created equal? Certainly not. Do you need high-quality salt for your body to function? Definitely. And eating salt that has natural minerals, including potassium, magnesium, and zinc, is a smart choice. Micronutrients often need partners to effectively allow your body to utilize them. Calcium needs vitamin D to help your body absorb it. Similarly, vitamin C can help aid in iron absorption. When sodium is paired with potassium, the potassium helps diminish any potentially troublesome effects of the sodium by influencing your kidneys to excrete the excess. Sodium and potassium aren’t just minerals and micronutrients, but are necessary electrolytes that your body needs to function. Interestingly, patients with hypothyroidism had significantly lower sodium levels than control groups, which can lead to electrolyte imbalance. This is why finding an unadulterated salt with natural minerals to use in your diet is important for your thyroid, as well as your overall health. Choose unrefined sea salt (made from evaporating seawater), or salt mined from deposits with minerals intact (those are the natural colors in the salt), unbleached, and a company that regularly does third-party testing for chemical contaminants, including heavy metals and microplastics.
The question must then be asked—If you’re not receiving iodine from iodized salt, where are you getting it? Seaweed is the most concentrated natural source of iodine you can find. One single gram of kombu kelp—thick and savory—provides up to 2000% of your Recommended Dietary Allowance (RDA), (approx 2984 mcg of iodine per gram of kombu), while the typical sushi seaweed, nori—thin, salty-sweet flavor—contains 16–43 mcg of iodine per gram of nori. Iodine poisoning can be a potential concern if small children consume more than 200 mcg (micrograms) daily, and adults more than 1,100 mcg. The recommended daily intake for iodine is 150 mcg for adults, and 120 mcg for children over 9 years old. If you do eat high-iodine foods, do so in moderation. Seaweed isn’t the only delicacy from the ocean to deliver the needed nutrients for your thyroid. Cod, shrimp, oysters, and tuna do so as well. And if seafood isn’t for you, one egg (24 mcg of iodine) and one cup of cottage cheese (65 mcg of iodine) can provide over half your daily needs of iodine. Vegetarian sources such as prunes, walnuts, and lima beans also contain small quantities. But with the amounts needed to achieve your iodine levels, the overload could amount to serious digestive distress.
As important as it is, iodine does not work alone. There are several minerals, that along with iodine are necessary for optimal thyroid function, including selenium and zinc. These minerals, in addition to others, are often found in sea salt. Selenium is particularly important because it is involved in the conversion of T4 (the inactive thyroid hormone) into T3 (the active form). Without adequate selenium, your body cannot efficiently convert T4 into T3, leading to low levels of active thyroid hormone and symptoms of hypothyroidism. Similarly, zinc is required for the synthesis of thyroid hormones and supports your immune system. Zinc deficiency has been linked to hypothyroidism, as it can inhibit the production of thyroid hormones and reduce your body’s ability to use them effectively. A deficiency in one or more of these minerals can exacerbate thyroid problems, particularly in the context of environmental toxicity or other stressors. Therefore, a balanced diet that includes adequate amounts of iodine, selenium, and zinc is essential for maintaining thyroid health.
The Impact on Your Thyroid From Chemicals in the Environment
Iodine's role isn't just about preventing deficiency, however, it’s also about protecting your thyroid from the onslaught of environmental toxins. In recent years, the prevalence of thyroid dysfunction has been linked to a variety of environmental toxins, including heavy metals, endocrine-disrupting chemicals (EDCs), and pesticides. Many of these substances interfere with thyroid hormone production, and their presence in food, water, air, and personal care products has become an alarming concern for thyroid health. EDCs are a broad category of chemicals that create chaos within the body’s hormonal systems, and are especially dangerous to the thyroid. These chemicals mimic, block, or alter the way thyroid hormones function. As a matter of fact, the toxic chemicals bromine, chlorine, and fluorine (fluoride) are all in the same group of halogens on the periodic table as iodine. Since these different elements are chemically similar, the thyroid can mistake one for the other leading to more problems with deficiency, as well as drenching your thyroid with their inherent toxicity. Other toxins and EDCs that can affect your thyroid include the following:
Polychlorinated biphenyls (PCBs): Once used in electrical equipment, these persistent pollutants have been associated with thyroid dysfunction, particularly in populations with high levels of exposure.
Bisphenol A (BPA): Found in plastics, BPA is a potent endocrine disruptor. Studies have shown that BPA can interfere with thyroid hormone levels and may contribute to thyroid disease.
Perfluorooctanoic acid (PFOA): Used in nonstick cookware, water-resistant fabrics, and firefighting foam, PFOA has been shown to affect thyroid function, leading to both hypothyroidism and hyperthyroidism in certain studies.
Pesticides: Various pesticides, particularly organochlorines and organophosphates, can alter thyroid hormone levels. These chemicals are commonly used in agriculture, making their presence in food and water a growing problem. Some pesticides also contain heavy metals, compounding the toxicity.
These chemicals accumulate in the environment and enter your body through inhalation, ingestion, or skin contact, posing serious risks to the way your thyroid behaves. They may impair the ability of iodine to enter the gland, disrupt the synthesis of thyroid hormones, or cause thyroid tissue damage. Another set of environmental toxins that disrupt thyroid function are heavy metals, such as arsenic, lead, mercury, and cadmium. These metals interfere with your thyroid gland’s ability to absorb iodine and produce thyroid hormones. For example, mercury exposure has been shown to disrupt thyroid hormone production and increase the risk of autoimmune thyroid diseases (Hashimoto’s disease: hypothyroid and Graves’ disease: hyperthyroid). Graves’ disease along with inflammation of the thyroid caused by viral infections are the most common causes of an overactive thyroid.
You can also develop hyperthyroidism from taking too much thyroid medication. Lead, which has been linked to cognitive impairments, may also disrupt thyroid function by blocking iodine uptake. Research suggests that environmental contamination by heavy metals is increasingly contributing to iodine deficiency and thyroid dysfunction. In populations with higher levels of heavy metal exposure (such as people that work or live near mines, refineries, petrochemical plants, chemical or pesticide production/application, and coal burning power stations), iodine supplementation and thyroid support may be particularly necessary to fight these harmful conditions.
Luckily, iodine is known to have protective effects against certain environmental chemicals. For example, research suggests that iodine may help counteract the thyroid-disrupting effects of heavy metals and EDCs by improving the thyroid's ability to produce hormones despite toxic exposure. This is because iodine directly supports the thyroid’s function, helping to maintain adequate hormone levels even in the face of environmental stressors. But that isn’t all … Iodine is a potent detoxifying agent as well. It helps your body eliminate harmful substances, including heavy metals and environmental pollutants. This detoxification extends to the thyroid, where iodine may assist in clearing out toxic chemicals that damage thyroid cells or interfere with hormone production. In a PubMed article, “Potential Effects of Iodine Supplementation on Inflammatory Processes and Toxin Removal Following COVID-19 Vaccination,” the author illustrates this point:
“Iodine binds well to toxins. Iodine also binds to metals such as aluminum and mercury. Iodine also helps thyroid functions, thus further contributing to detoxification.”
Additionally, iodine’s role in your body’s overall detoxification process can help protect other organs from the cumulative burden of toxins, further supporting thyroid function by reducing the toxic load on the entire endocrine system. Heavy metals and environmental toxins aren’t the only source of hormone disruption. Physiologist, Dr. Ray Peat asserts that seed oils which are full of polyunsaturated fatty acids (PUFAs), particularly linoleic acid, negatively impact thyroid function. They lower thyroid hormone levels resulting in metabolic dysfunction, which directly impacts your weight and health. A study performed 13 years ago, “Anti-Throid Effects Of Pufas (Polyunsaturated Fats) And Herbs,” published in the Trakya University Journal of Natural Sciences shows that research indicating the detrimental relationship between PUFAs and the thyroid is nothing new:
“When large amounts of PUFAs are consumed, they are stored and between meals, they are released. They poison the mitochondria, impair communication within the cell, impair the action of enzymes that dissolve blood clots and digest dietary protein, and inhibit the thyroid.”
Be Your Own Best Asset
While it is imperative to examine your current diet to identify potential threats to your thyroid health (like seed oils), you must also ensure you are getting the nutrition you need to nourish your thyroid in the first place. If you have thyroid issues, you may choose to avoid soy, gluten, and cruciferous vegetables, including kale. From HealthCentral, “Can Kale Cause Hypothyroidism?”
“These vegetables ‘“contain the substance thiocyanate, which in very high concentrations can interfere with adequate iodine nutrition,”’ says Angela M. Leung, M.D., an endocrinologist and clinical assistant professor of medicine at UCLA David Geffen School of Medicine, Los Angeles, and chair of the Public Health Committee at the American Thyroid Association.
The thyroid needs iodine to produce thyroid hormone, and ‘“thus exposure to very high amounts of thiocyanate can potentially result in hypothyroidism (an underactive thyroid) and compensatory growth of the thyroid (goiter),”’ Dr. Leung explains.”
Furthermore, if you are unable to meet your daily allowance of iodine through diet alone, you may decide to consider supplementation. Lugol’s iodine, which was first formulated in the 19th century by the French physician, Lugol, is emerging as one of the safer ways to supplement and support the thyroid. It is a solution of elemental iodine and potassium iodide in water taken by the drop. Even if you have a clinical diagnosis of hypothyroidism and are taking medications such as Synthroid (levothyroxine: a synthetic thyroid hormone) or Armour Thyroid (animal-derived source), you may find that supplementing with a high-quality iodine can help reduce or eliminate your need for medication. When choosing an iodine supplement, look for clearly labeled ingredients, avoid unnecessary additives, and ensure it’s third-party tested for contaminants, ideally with a certificate of analysis. If you are in a position where you need to take medication for your thyroid, and want to find a more natural and sustainable treatment plan, please consult with an integrative practitioner—perhaps a highly-skilled naturopathic or functional medicine doctor.
This team of professionals can help you bridge the gap between conventional medical knowledge and “whole-body” philosophy, to best guide you on your health path. If you suspect you may have a deficiency in iodine, or in your thyroid’s production, you may want to have your doctor run blood work to test for these markers. A conventional medical doctor and a holistic doctor will typically have vastly different approaches to treatment, so choose a medical team that will support your goals, values, and emotional landscape. The Weston A. Price Foundation (WAPF) offers sound advice when the time comes to seek out a diagnosis from medical professionals. From “A Successful Approach to Underactive Thyroid Hormone Function”:
“The only way to be sure that no form of hypothyroidism is present, when the patient exhibits suspicious symptoms of hypothyroidism, is to always measure the free-T3 serum level (preferably by the new, more accurate dialysis method) and the free-T4 level, in addition to the TSH level. When a low free-T3 level is not suspected or measured for, it will not be found, reinforcing the perception that low T3 levels, without abnormal T4 and TSH levels, are rare or insignificant. If the FT3 level is always measured, whenever thyroid function is tested, it will be found that a low T3 level is a common condition, leading to a lot of illness and death, while the patient is told that their thyroid function is normal (just because the TSH level, and perhaps a T4 level, is normal).”
Knowing what you want from your doctor before you arrive at their office is important. It’s necessary to be a strong advocate (and/or bring one with you) for your own care to get support in the direction you desire. In addition to running levels on TSH (thyroid-stimulating hormone; signals the thyroid to produce and release thyroid hormones), you can also request that free T4 (the amount of thyroxine in the blood not attached to proteins), free T3 (the amount of triiodothyronine in the blood not attached to proteins) and thyroid peroxidase AB (measures antibodies produced in the blood caused by damage to the thyroid) levels are checked. This will allow both you and your practitioner an opportunity to pinpoint potential problems without overlooking these vital markers.
The relationship between iodine, thyroid health, environmental factors, and nutrition is a complex and multifaceted one. Iodine is undoubtedly essential for the production of thyroid hormones, and also plays a critical role in protecting your thyroid. Today, with the avalanche of environmental pollutants in the air, water, and food, coupled with toxic PFAS “forever chemicals,” endocrine disruptors, heavy metals, and nutrient deficiencies, increasing natural sources of iodine, and/or supplementing with iodine, remain the beacon of hope for your thyroid health. While iodine may be integrally linked to healthy thyroid performance, do not underestimate the power of minerals to help facilitate this.
~
If you've found value in this article, please cross-post and restack it!
To support the research and health education of AVFC editorial, please consider making a donation today. Thank you.